Portal Venous Stenting for Portal Vein Anastomotic Stenosis After Liver Transplantation: A Case Report
Main Article Content
Abstract
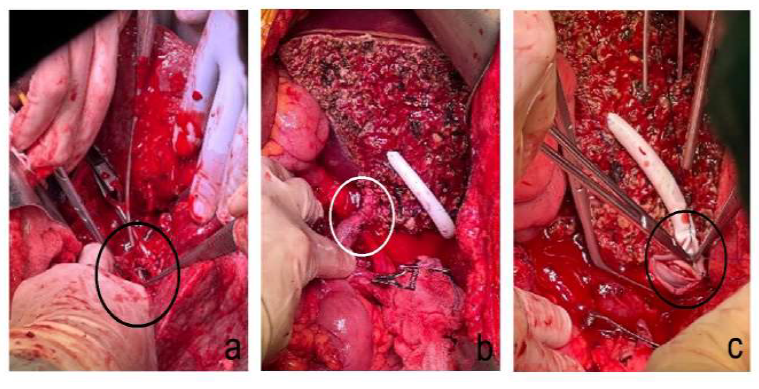
Liver transplantation (LT) is currently one of the most crucial methods for treating end-stage liver disease. The survival rate after transplantation has exceeded 70-80%. Vascular complications after LT are a significant cause of postoperative failure. Therefore, early diagnosis and proactive treatment of vascular complications after LT can lead to a more comprehensive recovery for the patient. This case involves a 55-year-old female patient with liver cirrhosis. Three days after the right lobe of the liver was transplanted, she was found to have elevated blood pressure, increased ascites, and deteriorating liver function. Doppler ultrasound revealed insufficient blood supply to the portal vein (PV), while computed tomography (CT) diagnosed stenosis at the PV anastomosis, resulting in partial thrombosis in the hepatic artery and hepatic vein. The self-expanding stent (Bard® E-LUMINEXX™) was deployed using angiography to widen the vascular anastomotic stenosis. The portal venogram after the stent placement revealed that the stent was well positioned and open, leading to improved PV flow and a significant reduction in PV pressure. Reduce pulse pressure and improve arterial blood flow.
Article Details
References
Gheorghe, G., Diaconu, C. C., Bungau, S., Bacalbasa, N., Motas, N., & Ionescu, V. A. (2023). Biliary and Vascular Complications after Liver Transplantation-From Diagnosis to Treatment. Medicina (Kaunas, Lithuania), 59(5), 850. https://doi.org/10.3390/medicina59050850
Bircher J, Benhamou JP, McIntyre N, Rizzetto M, Rodes J, editors. Oxford Textbook of Clinical Hepatology. 2nd Edition Oxford University Press; 1999.
Sherlock S, Dooley J, editors. Diseases of the Liver and Biliary System. 11th Edition Blackwell Science; Oxford, UK; Malden, MA: 2002.11. Gökçe AM, Kaya C, Kara VM, Ozel L, Ruhi C, Titiz MI. (2015) Effects of urethral stricture on allografts in kidney transplantation. Transplant Proc, 47(5), 1336–9. https://doi.org/10.1016/j.transproceed.2015.04.072.
Schiff ER, Sorrell MF, Maddrey EC, editors. Schiff’s Diseases of the Liver. 9th Edition Lippincott, Williams & Wilkins; Philadelphia: 2003.
Bengtsson B, Widman L, Wahlin S, Stål P, Björkström NK, Hagström H. The risk of hepatocellular carcinoma in cirrhosis differs by etiology, age and sex: a Swedish nationwide population-based cohort study. United European Gastroenterol J. 2022; 10(5): 465–76. https://doi.org/10.1002/ueg2.12238
Piardi T, Lhuaire M, Bruno O, Memeo R, Pessaux P, Kianmanesh R, Sommacale D. Vascular complications following liver transplantation: A literature review of advances in 2015. World J Hepatol 2016; 8(1): 36-57 URL: https://www.wjgnet.com/1948-5182/full/v8/i1/36.htm DOI: https://dx.doi.org/10.4254/wjh.v8.i1.36
Gheorghe, G., Diaconu, C. C., Bungau, S., Bacalbasa, N., Motas, N., & Ionescu, V. A. (2023). Biliary and Vascular Complications after Liver Transplantation-From Diagnosis to Treatment. Medicina (Kaunas, Lithuania), 59(5), 850. https://doi.org/10.3390/medicina59050850
Nemes, B., Gámán, G., Polak, W. G., Gelley, F., Hara, T., Ono, S., Baimakhanov, Z., Piros, L., & Eguchi, S. (2016). Extended-criteria donors in liver transplantation Part II: reviewing the impact of extended-criteria donors on the complications and outcomes of liver transplantation. Expert review of gastroenterology & hepatology, 10(7), 841–859. https://doi.org/10.1586/17474124.2016.1149062
Funaki B, Rosenblum JD, Leef JA, Hackworth CA, Szymski GX, Alonso EM, Piper JB, Whitington PF. Portal vein stenosis in children with segmental liver transplants: treatment with percutaneous transhepatic venoplasty. AJR Am J Roentgenol. 1995;165:161-165.
Jeon, U. B., Kim, C. W., Kim, T. U., Choo, K. S., Jang, J. Y., Nam, K. J., Chu, C. W., & Ryu, J. H. (2016). Therapeutic efficacy and stent patency of transhepatic portal vein stenting after surgery. World journal of gastroenterology, 22(44), 9822–9828.
Funaki B, Rosenblum JD, Leef JA, Hackworth CA, Szymski GX, Alonso EM. Angioplasty treatment of portal vein stenosis in children with segmental liver transplants: mid-term results. AJR Am J Roentgenol. 1997;169:551-554.
Raby N, Karani J, Thomas S, O’Grady J, Williams R. Stenoses of vascular anastomoses after hepatic transplantation: treatment with balloon angioplasty.
AJR Am J Roentgenol. 1991;157:167-171.
Jia, Y. P., Lu, Q., Gong, S., Ma, B. Y., Wen, X. R., Peng, Y. L., Lin, L., Chen, H. Y., Qiu, L., & Luo, Y. (2007). Postoperative complications in patients with portal vein thrombosis after liver transplantation: evaluation with Doppler ultrasonography. World journal of gastroenterology, 13(34), 4636–4640. https://doi.org/10.3748/wjg.v13.i34.4636
Copelan, A., George, D., Kapoor, B., Nghiem, H. V., Lorenz, J. M., Erly, B., & Wang, W. (2015). Iatrogenic-related transplant injuries: the role of the interventional radiologist. Seminars in interventional radiology, 32(2), 133–155. https://doi.org/10.1055/s-0035-1549842
Akgul, E., Inal, M., Soyupak, S., Binokay, F., Aksungur, E., & Oguz, M. (2002). Portal venous variations. Prevalence with contrast-enhanced helical CT. Acta radiologica (Stockholm, Sweden : 1987), 43(3), 315–319. https://doi.org/10.1080/j.1600-0455.2002.430314.x