Incidence of Adverse Effects Associated with Strong Opioids Treatment for Oncological Pain
Main Article Content
Abstract
Background: Opioids are the most commonly drugs used in oncological pain treatment due to its potency and availability and the mechanism underlying their adverse effects is secondary to the activation of the subtypes of opioids receptors. The incidence of adverse effects due opioid treatment varies according on the population, drug dosage and individual comorbidities, being the most common ones: Constipation, nausea and vomiting, dyspnea, drowsiness and opioid use disorder. The presence of adverse effects may be crucial in the context of treatment failure, the goal of this research is to report the incidence of adverse effects associated with the use of strong opioids in diagnosed cancer population.
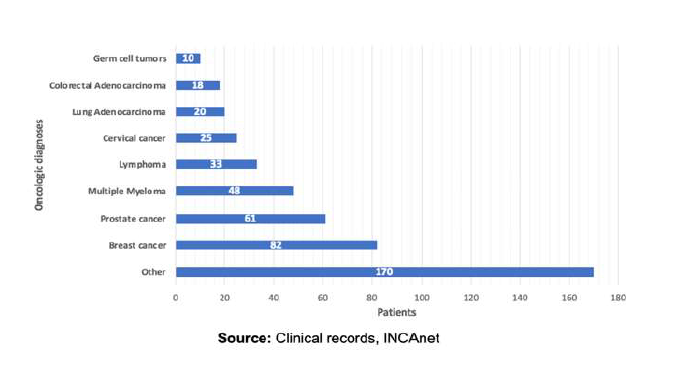
Materials and methods: This research is conducted with outpatients from the “Instituto nacional de cancerología”, the national reference center of oncology in Mexico, from march to september 2023. From the total of 1230 cases that were reviewed, 467 of them met the inclusion criteria. We consider as strong opioids: Morphine, Buprenorphine, Tapentadol, Oxycodone, Fentanyl and Methadone. For the assessment of the incidence of adverse effects, we employ the Edmonton Symptom Assessment Scale, which is standardized on a numerical scale ranging from 0 to 10 points based on the intensity of the adverse effects.
Results: In the studied sample, 59,1% are women. The mean age is 57,6 ± 13,7 years with a mean BMI of 26,5 ± 5,8 kg/m2. The most common adverse effect associated with the use of opioids in cancer patients is constipation, occurring in 25,9% of the cases, followed by nausea and vomiting at 19,1%, respiratory depression at 1,7%, erythema at 1,3% and drowsiness at 1,3%. Fentanil shows the highest incidence of adverse effects, with constipation occurring in 46,7% of cases and nausea and vomiting at 26,7%. Oxycodone follows closely behind with a 41,7% incidence rate for both variables.
Conclusion: The adverse effects in order or frequency were: Constipation, nausea and vomiting, respiratory depression, erythema and drowsiness, exhibiting a minor incidence compared to other reviews. This enables us to understand the influence of our treatments and the precautions to consider in order to prevent an adverse effect from being the cause of opioid treatment failure, especially in oncologic patients with refractory pain.
Article Details
References
Machelska H, Celik MÖ. Advances in Achieving Opioid Analgesia Without Side Effects. Frontiers in Pharmacology [Internet]. 2018;9. doi: 10.3389/fphar.2018.01388.
Eriksson LI., Fleisher LA., Wiener-Kronish JP. Miller’s Anesthesia [Internet]. 2020. Available from: http://books.google.ie/books?id=IDUwzAEACAAJ&dq=9780323612630&hl=&cd=1&source=gbs_api.
Manchikanti L, Manchikanti KN, Kaye AD, Kaye AM, Hirsch JA. Challenges and concerns of persistent opioid use in cancer patients. Expert Review of Anticancer Therapy [Internet]. 2018;18:705–718. doi: 10.1080/14737140.2018.1474103.
Salvetti M de G, Machado CSP, Donato SCT, Silva AM da. Prevalence of symptoms and quality of life of cancer patients. Revista Brasileira de Enfermagem [Internet]. 2020;73. doi: 10.1590/0034-7167-2018-0287.
Nelson AD, Camilleri M. Opioid-induced constipation: advances and clinical guidance. Therapeutic Advances in Chronic Disease [Internet]. 2016;7:121–134. doi: 10.1177/2040622315627801.
Mearin F, Ciriza C, Mínguez M, Rey E, Mascort JJ, Peña E, Cañones P, Júdez J. Guía de práctica clínica: síndrome del intestino irritable con estreñimiento y estreñimiento funcional en adultos: concepto, diagnóstico y continuidad asistencial. (Parte 1 de 2). Atención Primaria [Internet]. 2017;49:42–55. doi: 10.1016/j.aprim.2016.11.003.
Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Adult Cancer Pain V.2.2023. © National Comprehensive Cancer Network, Inc. 2023. All rights reserved. Accessed [January 27, 2024]. To view the most recent and complete version of the guideline, go online to NCCN.org.
Sande TA, Laird BJA, Fallon MT. The Management of Opioid-Induced Nausea and Vomiting in Patients with Cancer: A Systematic Review. Journal of Palliative Medicine [Internet]. 2019;22:90–97. doi: 10.1089/jpm.2018.0260.
Mallick‐Searle T, Fillman M. The pathophysiology, incidence, impact, and treatment of opioid‐induced nausea and vomiting. Journal of the American Association of Nurse Practitioners [Internet]. 2017;29:704–710. doi: 10.1002/2327-6924.12532.
Lee LA, Caplan RA, Stephens LS, Posner KL, Terman GW, Voepel-Lewis T, Domino KB. Postoperative Opioid-induced Respiratory Depression. Anesthesiology [Internet]. 2015;122:659–665. doi: 10.1097/aln.0000000000000564.
van der Schier R, Roozekrans M, van Velzen M, Dahan A, Niesters M. Opioid-induced respiratory depression: reversal by non-opioid drugs. F1000Prime Reports [Internet]. 2014;6. doi: 10.12703/p6-79.
1. Del Vecchio G, Spahn V, Stein C. Novel Opioid Analgesics and Side Effects. ACS Chemical Neuroscience [Internet]. 2017;8:1638–1640. doi: 10.1021/acschemneuro.7b00195.
Khademi H, Kamangar F, Brennan P, Malekzadeh R. Opioid Therapy and its Side Effects: A Review. Arch Iran Med [Internet]. 2016 Dec;19(12):870-876. PMID: 27998163.
Calvo Falcón R, Torres Morera L miguel. Tratamiento con opiodes en dolor crónico no oncológico: Recomendaciones para una prescripción segura. Revista de la Sociedad Española del Dolor [Internet]. 2017; doi: 10.20986/resed.2017.3550/2016.
Oldenmenger WH, de Raaf PJ, de Klerk C, van der Rijt CCD. Cut Points on 0–10 Numeric Rating Scales for Symptoms Included in the Edmonton Symptom Assessment Scale in Cancer Patients: A Systematic Review. Journal of Pain and Symptom Management [Internet]. 2013;45:1083–1093. doi: 10.1016/j.jpainsymman.2012.06.007.
Paice JA, Portenoy R, Lacchetti C, Campbell T, Cheville A, Citron M, Constine LS, Cooper A, Glare P, Keefe F, et al. Management of Chronic Pain in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. Journal of Clinical Oncology [Internet]. 2016;34:3325–3345. doi: 10.1200/jco.2016.68.5206.
Henschke N, Kamper SJ, Maher CG. The Epidemiology and Economic Consequences of Pain. Mayo Clinic Proceedings [Internet]. 2015;90:139–147. doi: 10.1016/j.mayocp.2014.09.010.
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, Znaor A, Bray F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. International Journal of Cancer [Internet]. 2018;144:1941–1953. doi: 10.1002/ijc.31937.
Zajączkowska R, Kocot-Kępska M, Leppert W, Wordliczek J. Bone Pain in Cancer Patients: Mechanisms and Current Treatment. International Journal of Molecular Sciences [Internet]. 2019;20:6047. doi: 10.3390/ijms20236047.
Allen KB, Brovman EY, Chhatriwalla AK, Greco KJ, Rao N, Kumar A, Urman RD. Opioid-Related Adverse Events: Incidence and Impact in Patients Undergoing Cardiac Surgery. Seminars in Cardiothoracic and Vascular Anesthesia [Internet]. 2019;24:219–226. doi: 10.1177/1089253219888658.
Mercadante S. Opioid Analgesics Adverse Effects: The Other Side of the Coin. Current Pharmaceutical Design [Internet]. 2019;25:3197–3202. doi: 10.2174/1381612825666190717152226.
Paul AK, Smith CM, Rahmatullah M, Nissapatorn V, Wilairatana P, Spetea M, Gueven N, Dietis N. Opioid Analgesia and Opioid-Induced Adverse Effects: A Review. Pharmaceuticals [Internet]. 2021;14:1091. doi: 10.3390/ph14111091.
McNicol E, Horowicz-Mehler N, Fisk RA, Bennett K, Gialeli-Goudas M, Chew PW, Lau J, Carr D. Management of opioid side effects in cancer-related and chronic noncancer pain: a systematic review. The Journal of Pain [Internet]. 2003;4:231–256. doi: 10.1016/s1526-5900(03)00556-x.